IgM-associated gut bacteria in obesity and type 2 diabetes in C57BL/6 mice and humans – published online 19/05/2022
James A. Pearson, Heyuan Ding, Changyun Hu, Jian Peng, Brittany Galuppo, F. Susan Wong, Sonia Caprio, Nicola Santoro, Li Wen
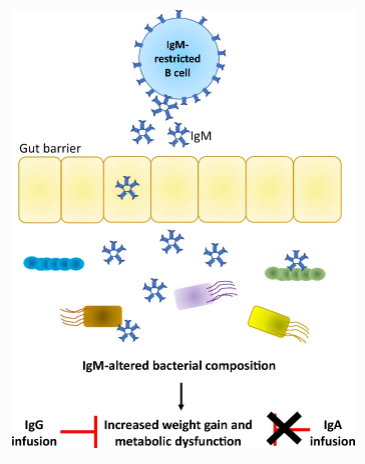
B cells secrete different immunoglobulins, which can target bacteria. IgA-deficiency promotes obesity through changes to the composition of gut bacteria; however, IgA deficiency often increases IgM. In this issue, Pearson, Ding and Hu et al (https://doi.org/10.1007/s00125-022-05711-8) used activation-induced cytidine deaminase (AID)-deficient mice (which produce only IgM) fed on a high fat diet to investigate the role of IgM in obesity. They show that increased IgM promoted weight gain and impaired glucose- and insulin tolerance by altering the composition of the intestinal bacteria in the mice. Administration of intravenous IgG, but not IgA, abolished the obesogenic profile of AID-deficient mice. The authors also showed that in obese children with impaired glucose tolerance and type 2 diabetes, IgM-bound stool bacteria are increased compared with normoglycaemic children without type 2 diabetes. Additionally, gut bacteria derived from either AID-deficient obese mice or obese children with impaired glucose tolerance and type 2 diabetes induced similar metabolic changes in germ-free mice. The authors conclude that these findings indicate that IgM may be important in the development of obesity and type 2 diabetes.
All News